Dr Ahsan Tariq , MBBS, MRCP (UK ) ongoing, IMT ( Internal Medicine Trainee, NHS England), GMC : 7805049
Dr Ahsan Tariq is a UK-registered medical doctor with a background in internal medicine and a focus on evidence-based research in cognitive health and nootropics. He critically reviews scientific studies, supplements, and ingredients to help readers make informed, safe, and effective choices for brain health and performance.
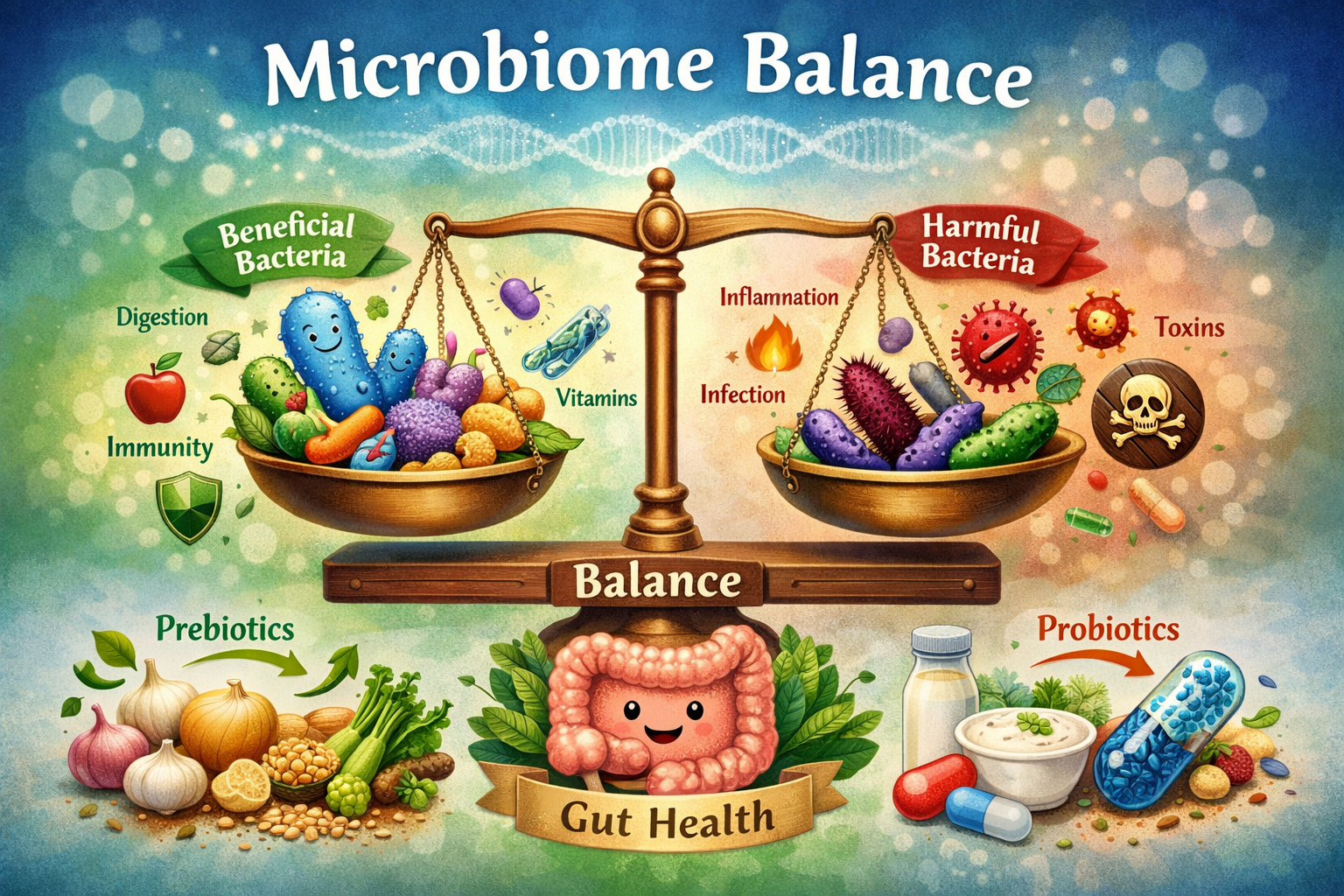
Introduction: Why Microbiome Balance Matters Today
The human microbiome refers to the trillions of microorganisms bacteria, viruses, fungi, and archaea that live in and on the human body, with the largest and most influential population residing in the gastrointestinal tract. Over the past two decades, advances in genomic sequencing and bioinformatics have transformed microbiome research from a niche scientific interest into a central pillar of modern health science. According to large-scale sequencing projects, including the Human Microbiome Project, microbiome balance is closely associated with digestive efficiency, immune regulation, metabolic stability, and even neurological signaling [1].
Microbiome balance does not mean the absence of harmful bacteria; rather, it reflects a dynamic equilibrium where beneficial microbes dominate, pathogenic organisms are kept in check, and overall diversity remains high. When this balance is disrupted a condition known as dysbiosis research consistently links it to inflammation, chronic disease, and reduced resilience to environmental stressors [2].
This article provides a comprehensive, theory-driven exploration of microbiome balance research. It moves systematically from foundational awareness to proven benefits and finally to real scientific concerns and limitations. Drawing on peer-reviewed studies, clinical observations, and population-level research, the discussion is designed to support clear understanding, critical thinking, and evidence-based decision-making.
Understanding The Human Microbiome
What Is Microbiome Balance?
Microbiome balance refers to a stable and functionally diverse microbial ecosystem within the gut. Research emphasizes that balance is defined less by the presence of specific bacterial species and more by overall diversity, functional redundancy, and metabolic cooperation among microbes [3]. A balanced microbiome can adapt to dietary changes, resist pathogenic invasion, and communicate effectively with host systems.
Studies comparing healthy individuals with those experiencing chronic illness consistently show that reduced microbial diversity and altered metabolic output are hallmarks of imbalance [4]. This has positioned microbiome balance as a measurable indicator of overall physiological resilience.
How The Microbiome Develops Across The Lifespan
Microbiome development begins at birth and continues to evolve throughout life. Mode of delivery, early feeding practices, antibiotic exposure, and environmental contact all shape initial microbial colonization [5]. During childhood, microbial diversity increases rapidly, stabilizing in early adulthood.
Although relatively stable in adults, the microbiome remains sensitive to long-term dietary patterns, stress, illness, and medication use. Aging is also associated with shifts in microbial composition, some of which correlate with increased inflammation and reduced immune function [6].
Core Functions Of A Balanced Microbiome
A balanced microbiome performs several essential functions:
- Breakdown of complex carbohydrates and dietary fiber
- Production of short-chain fatty acids (SCFAs)
- Regulation of immune cell development
- Maintenance of gut barrier integrity
- Modulation of hormonal and neurological pathways
Experimental and clinical studies demonstrate that these functions are compromised during dysbiosis, reinforcing the importance of microbial balance for systemic health [7].
Microbiome Balance And Digestive Health
Role In Digestion And Nutrient Metabolism
Human digestive enzymes cannot fully break down many plant-based compounds. Gut microbes ferment these substrates, producing SCFAs such as acetate, propionate, and butyrate. According to metabolic research, SCFAs serve as energy sources for intestinal cells and help regulate inflammation and glucose metabolism [8].
Association With Digestive Disorders
Microbiome imbalance is strongly associated with digestive disorders including irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and functional dyspepsia. A comprehensive meta-analysis reported significantly altered microbial profiles in individuals with IBS compared to healthy controls [9].
Gut Barrier Integrity And Inflammation
A balanced microbiome supports the integrity of the intestinal barrier. Dysbiosis may increase intestinal permeability, allowing microbial byproducts to enter systemic circulation and trigger inflammation. This mechanism has been documented in both animal models and human clinical studies [10].
Immune System Regulation And Microbiome Balance
Microbiome–Immune System Crosstalk
Approximately 70% of the body’s immune cells are located in the gut. The microbiome plays a central role in educating these immune cells, helping them differentiate between harmful pathogens and harmless antigens [11]. Balanced microbial exposure promotes immune tolerance and reduces inappropriate inflammatory responses.
Autoimmune And Allergic Conditions
Epidemiological studies reveal consistent associations between altered gut microbiota and autoimmune conditions such as type 1 diabetes, multiple sclerosis, and rheumatoid arthritis [12]. Early-life microbiome disruption appears particularly influential in shaping long-term immune outcomes.
Protection Against Infections
A healthy microbiome provides colonization resistance by competing with pathogens for nutrients and attachment sites. Hospital-based studies show that microbiome disruption increases susceptibility to infections such as Clostridioides difficile [13].
Microbiome Balance And Metabolic Health
Energy Harvest And Weight Regulation
Gut microbes influence how efficiently calories are extracted from food. Comparative studies between lean and obese individuals demonstrate distinct microbial signatures, suggesting a role in weight regulation and fat storage [14].
Insulin Sensitivity And Metabolic Inflammation
Clinical trials indicate that greater microbial diversity is associated with improved insulin sensitivity and reduced markers of metabolic inflammation [15]. These findings highlight the microbiome as a modifiable factor in metabolic health.
Cardiovascular Risk Factors
Certain gut bacteria metabolize dietary components into compounds that influence cardiovascular risk. Research shows both protective and potentially harmful pathways, underscoring the complexity of microbiome–heart interactions [16].
Mental Health And The Gut–Brain Axis
Biological Pathways Of The Gut–Brain Axis
The gut–brain axis involves bidirectional communication through neural, immune, and endocrine pathways. Microbial metabolites can influence neurotransmitter production and stress hormone regulation [17].
Effects On Mood And Stress Regulation
Animal studies and early human trials suggest that microbiome composition affects stress reactivity and emotional behavior. However, researchers caution that human evidence remains correlational rather than causal [18].
Cognitive Health And Neurodevelopment
Emerging research explores links between microbiome balance and cognitive aging, neurodevelopment, and neurodegenerative conditions. Long-term, large-scale human studies are still needed to confirm these associations [19].
Proven Benefits Of Supporting Microbiome Balance
Evidence-Based Health Gains
Research-supported benefits of microbiome balance include improved digestive efficiency, enhanced immune resilience, reduced chronic inflammation, and improved metabolic regulation. A systematic review confirmed consistent associations between microbial diversity and positive health markers [20].
Dietary Patterns With Strong Evidence
High-fiber diets, diverse plant intake, and fermented foods are repeatedly linked with healthier microbiome profiles across populations [21]. These findings are among the most consistent in microbiome research.
Real Concerns And Scientific Limitations
Probiotic Overgeneralization
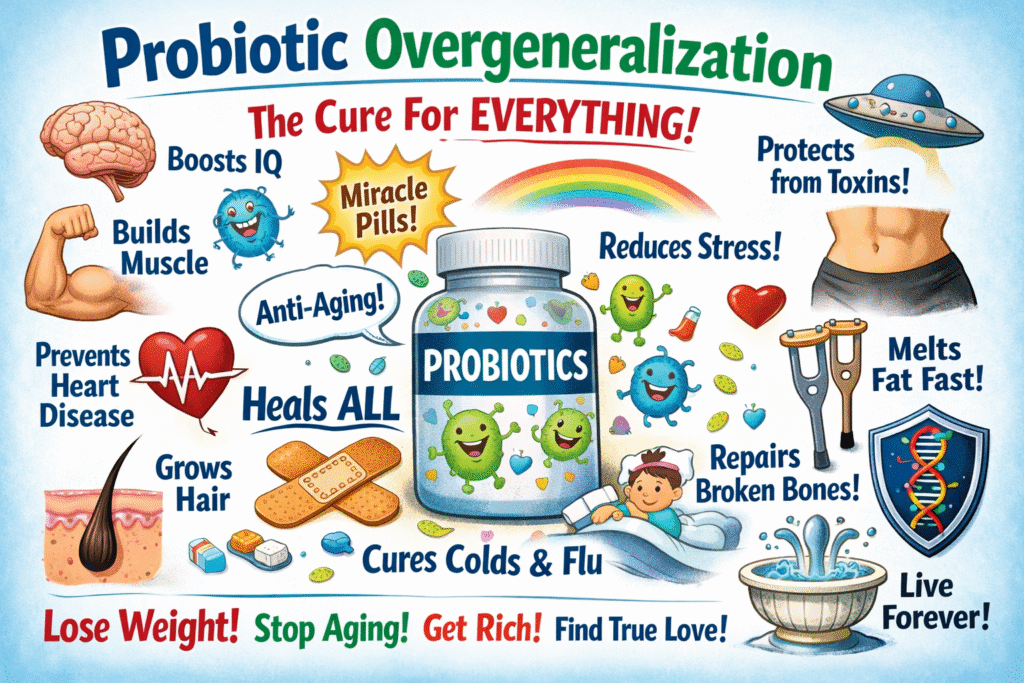
Although probiotics are widely marketed, evidence shows they are not universally beneficial. Some studies suggest probiotics may delay natural microbiome recovery following antibiotic use [22].
Individual Variability And Precision Challenges
Microbiome composition varies widely between individuals due to genetics, diet, and environment. This variability limits standardized recommendations and highlights the need for personalized approaches [23].
Gaps In Long-Term Human Research
Many microbiome studies are short-term or observational. Experts emphasize the need for long-term randomized controlled trials to establish causality [24].
Factors That Disrupt Microbiome Balance
Antibiotic And Medication Effects
Antibiotics can drastically reduce microbial diversity. Recovery may take months and is sometimes incomplete, particularly after repeated exposure [25].
Diet, Stress, And Lifestyle Factors
Highly processed diets, chronic psychological stress, physical inactivity, and poor sleep patterns are consistently associated with dysbiosis [26].
Environmental Influences
Urban living, reduced exposure to natural environments, and chemical pollutants may also contribute to microbiome disruption [27].
Strategies To Support Microbiome Balance
Nutrition-Based Strategies
Whole-food diets rich in fiber, polyphenols, and diverse plant sources are strongly supported by evidence [28].
Lifestyle And Behavioral Factors
Regular physical activity, stress management, and adequate sleep contribute to microbial stability and diversity [29].
Clinical And Medical Considerations
For individuals with chronic illness, microbiome-targeted interventions should be supervised by healthcare professionals to avoid unintended effects [30].
Summary Table: Proven Gains Vs Real Concerns
| Aspect | Proven Gains | Real Concerns |
|---|---|---|
| Digestive Health | Better digestion, SCFA production | High individual variability |
| Immune Function | Improved immune regulation | Limited causal evidence |
| Metabolic Health | Enhanced insulin sensitivity | Complex interactions |
| Mental Health | Gut–brain signaling support | Early-stage research |
Conclusion: A Balanced Interpretation Of Microbiome Research
Microbiome balance research offers compelling evidence that gut microbes play a central role in human health. At the same time, real scientific concerns such as individual variability, over-commercialization, and limited long-term data underscore the need for cautious interpretation. A theory-informed, evidence-based approach that emphasizes nutrition, lifestyle, and ongoing research remains the most reliable path forward.
References
- Human Microbiome Project Consortium (2012)
- Turnbaugh et al. (2007)
- Flint et al. (2012)
- Valdes et al. (2018)
- Dominguez-Bello et al. (2010)
- O’Toole & Jeffery (2015)
- Belkaid & Hand (2014)
- Koh et al. (2016)
- Pittayanon et al. (2019)
- Bischoff et al. (2014)
- Hooper et al. (2012)
- Vatanen et al. (2016)
- Buffie et al. (2015)
- Ley et al. (2006)
- Karlsson et al. (2013)
- Tang et al. (2017)
- Cryan & Dinan (2012)
- Foster et al. (2017)
- Sharon et al. (2016)
- Valdes et al. (2018)
- De Filippis et al. (2016)
- Suez et al. (2018)
- Zmora et al. (2018)
- Knight et al. (2017)
- Palleja et al. (2018)
- Sonnenburg & Sonnenburg (2019)
- Rook et al. (2017)
- Makki et al. (2018)
- Barton et al. (2018)
- Mullish et al. (2018)