Dr Ahsan Tariq , MBBS, MRCP (UK ) ongoing, IMT ( Internal Medicine Trainee, NHS England), GMC : 7805049
Dr Ahsan Tariq is a UK-registered medical doctor with a background in internal medicine and a focus on evidence-based research in cognitive health and nootropics. He critically reviews scientific studies, supplements, and ingredients to help readers make informed, safe, and effective choices for brain health and performance.
Introduction
Osteoporosis prevention is a critical public health priority as bone-related disorders continue to rise globally. Osteoporosis is a condition characterized by reduced bone density and structural deterioration, leading to fragile bones and an increased risk of fractures. While it is more common in older adults, especially postmenopausal women, osteoporosis often develops silently over many years. Preventive strategies implemented early in life can significantly reduce long-term fracture risk and preserve mobility, independence, and quality of life. This article provides a comprehensive, science-based guide to osteoporosis prevention, covering mechanisms, benefits, risks, evidence, and practical recommendations.
Understanding Osteoporosis Prevention
Osteoporosis prevention refers to a combination of lifestyle, nutritional, and medical strategies designed to maintain optimal bone mass and slow bone loss. Bone tissue is dynamic, constantly undergoing remodeling through bone formation and resorption. When bone breakdown exceeds bone formation, bone density declines, increasing fracture susceptibility [1]. Preventive measures aim to maximize peak bone mass during youth and minimize bone loss with aging.
How Osteoporosis Prevention Works
Bone Remodeling and Density Maintenance
Bone remodeling is regulated by osteoblasts, which build bone, and osteoclasts, which break it down. Preventive strategies support osteoblast activity while limiting excessive osteoclast action [2]. Adequate intake of calcium, vitamin D, protein, and micronutrients supports mineralization, while mechanical loading through exercise stimulates bone formation [3].
Hormonal and Lifestyle Influences
Hormones such as estrogen and testosterone play a key role in bone preservation. Declining estrogen levels after menopause accelerate bone loss, making prevention particularly important for women [4]. Lifestyle factors such as smoking, excessive alcohol intake, and physical inactivity negatively affect bone health [5].
Importance of Osteoporosis Prevention
Osteoporosis is responsible for millions of fractures worldwide each year, particularly of the hip, spine, and wrist [6]. Hip fractures are associated with increased mortality and long-term disability [7]. Preventing osteoporosis reduces healthcare costs, preserves independence, and lowers fracture-related morbidity [8].
Proven Benefits of Osteoporosis Prevention
Reduced Fracture Risk
Preventive strategies significantly reduce the risk of osteoporotic fractures by improving bone mineral density and strength [9].
Improved Mobility and Quality of Life
Maintaining bone health supports physical mobility, balance, and confidence in daily activities, reducing fall risk [10].
Long-Term Skeletal Health
Early prevention helps individuals achieve higher peak bone mass, providing a protective reserve against age-related bone loss [11].
Potential Risks and Limitations
Over-Supplementation
Excessive calcium supplementation may increase the risk of kidney stones and cardiovascular complications in some individuals [12].
Improper Exercise Techniques
High-impact or unsupervised resistance training may increase injury risk, particularly in individuals with existing bone loss [13].
Delayed Diagnosis
Relying solely on lifestyle measures without appropriate screening may delay detection of osteoporosis in high-risk individuals [14].
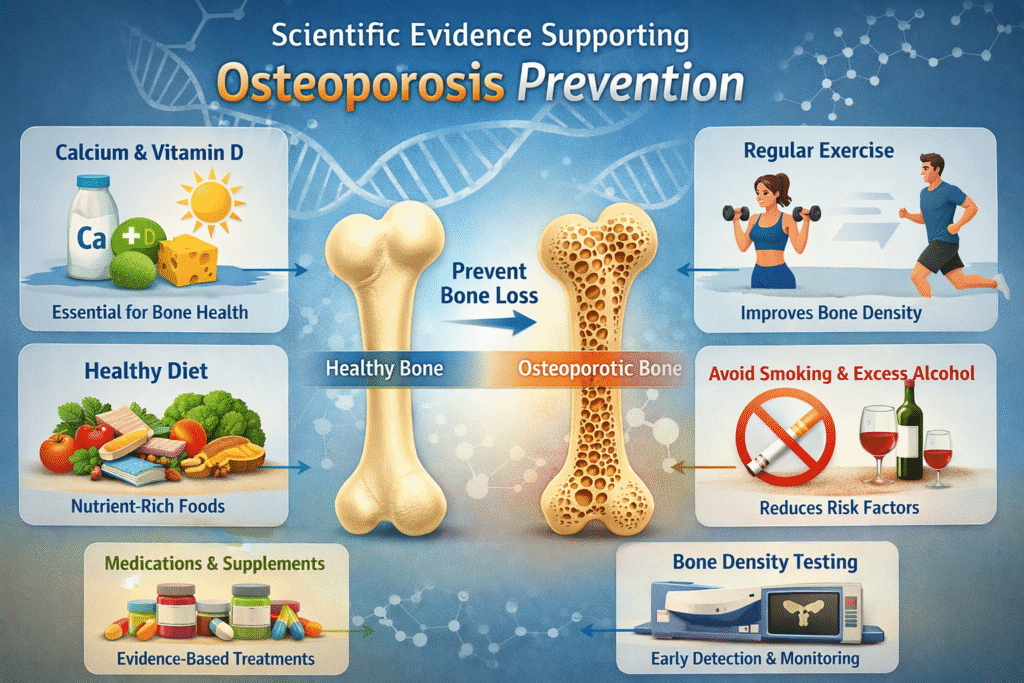
Scientific Evidence Supporting Osteoporosis Prevention
Extensive research supports preventive interventions. Weight-bearing exercise has been shown to improve bone density in both younger and older adults [15]. Adequate calcium and vitamin D intake is associated with reduced fracture incidence in elderly populations [16]. Longitudinal studies demonstrate that lifestyle modifications significantly slow age-related bone loss [17].
Comparison of Key Osteoporosis Prevention Strategies
| Strategy | Primary Benefit | Limitations |
|---|---|---|
| Calcium and vitamin D intake | Supports bone mineralization | Risk with excessive intake |
| Weight-bearing exercise | Stimulates bone formation | Requires consistency |
| Resistance training | Improves bone strength | Injury risk if unsupervised |
| Lifestyle modification | Reduces bone loss factors | Requires long-term adherence |
Benefits vs Risks of Osteoporosis Prevention
| Aspect | Benefits | Risks |
|---|---|---|
| Nutrition | Stronger bones, reduced fractures | Over-supplementation |
| Exercise | Increased bone density | Musculoskeletal injury |
| Screening | Early detection | Anxiety or overdiagnosis |
| Lifestyle changes | Overall health improvement | Behavioral challenges |
Safe Usage Guidelines for Osteoporosis Prevention
Individuals should aim for age-appropriate calcium and vitamin D intake as recommended by health authorities [18]. Exercise programs should include weight-bearing, balance, and resistance activities tailored to individual fitness levels [19]. Smoking cessation and moderation of alcohol intake are strongly advised [20]. Regular bone density screenings are recommended for high-risk populations [21].
Who Should Avoid Certain Preventive Approaches
People with kidney disease, hypercalcemia, or certain cardiovascular conditions should consult healthcare professionals before using calcium supplements [22]. Individuals with advanced osteoporosis should avoid high-impact exercises that increase fracture risk [23].
Alternatives and Complementary Approaches
Pharmacological therapies such as bisphosphonates may be considered for individuals at high fracture risk [24]. Nutritional approaches emphasizing whole foods rich in calcium, magnesium, and vitamin K provide additional support [25]. Fall-prevention programs and home safety modifications also reduce fracture risk [26].
Expert Opinions on Osteoporosis Prevention
Experts emphasize that prevention should begin early in life and continue throughout adulthood. According to leading endocrinologists, lifestyle-based prevention remains the foundation of bone health management [27]. Public health authorities recommend combining nutrition, exercise, and screening for optimal outcomes [28].
Key Takeaways
Osteoporosis prevention is most effective when started early and maintained consistently. A balanced diet, regular exercise, healthy lifestyle habits, and appropriate medical screening collectively reduce fracture risk and support long-term skeletal health.
Frequently Asked Questions
Can osteoporosis be completely prevented?
While not all cases can be prevented, preventive strategies significantly reduce risk and severity [29].
At what age should prevention begin?
Bone health strategies should begin in childhood and continue throughout life to maximize peak bone mass [30].
Is osteoporosis prevention only important for women?
No, men also experience bone loss with aging and benefit from preventive measures.
Conclusion
Osteoporosis prevention is a lifelong commitment that plays a crucial role in maintaining bone strength, reducing fracture risk, and preserving quality of life. Scientific evidence consistently supports the effectiveness of early intervention through nutrition, exercise, lifestyle modification, and screening. By adopting evidence-based preventive strategies, individuals can protect their skeletal health and reduce the personal and societal burden of osteoporosis.
References
- National Institutes of Health Osteoporosis Overview
- Bone Remodeling Mechanisms Review, 2014
- Wolff’s Law and Bone Adaptation Study, 2012
- Estrogen and Bone Loss Study, 2015
- Smoking and Bone Health Review, 2013
- International Osteoporosis Foundation Global Report
- Hip Fracture Mortality Analysis, 2016
- Economic Impact of Osteoporosis Study, 2018
- Fracture Prevention Meta-Analysis, 2017
- Mobility and Bone Health Study, 2014
- Peak Bone Mass Research Review, 2011
- Calcium Supplement Safety Review, 2016
- Exercise-Related Injury Risk Study, 2015
- Osteoporosis Screening Guidelines Review, 2019
- Weight-Bearing Exercise Clinical Trial, 2013
- Vitamin D and Fracture Risk Study, 2014
- Lifestyle and Bone Loss Longitudinal Study, 2012
- Dietary Reference Intakes for Calcium, 2011
- Exercise Prescription for Bone Health, 2018
- Alcohol Consumption and Bone Density Study, 2015
- Bone Density Testing Recommendations, 2020
- Calcium Supplement Contraindications Review, 2016
- Exercise Safety in Osteoporosis Study, 2017
- Pharmacologic Osteoporosis Prevention Review, 2018
- Micronutrients and Bone Health Review, 2014
- Fall Prevention and Fracture Reduction Study, 2016
- Endocrinology Expert Consensus, 2019
- World Health Organization Bone Health Guidelines
- Osteoporosis Risk Reduction Review, 2015
- Lifespan Bone Health Development Study, 2010

